Cannabis and Chronic Pain
Lori Kanter • October 1, 2022
Many Medical Patient’s use Cannabis to relieve pain, but how does it work? In this blog post, we’ll explore how cannabis can help relieve pain for medical patients
The treatment of pain remains the number one medical use of cannabis. 1 Using either THC or CBD to treat pain many additional factors need to be considered. Regarding pain there are phenotypic and genotypic interindividual variability 2 and different cannabinoids may lead to mechanistically different pain-relieving effects. 3
In addition, using cannabis in pain management can address disturbed sleep 4, anxiety and depression which often present as co- morbidities in pain.
Cannabis has been used for the treatment of pain dating back to Chinese texts in 2900 B.C. 5
The three main pain systems are nociceptive, neuropathic and central. Nociceptive pain is caused by damage to body tissues and is usually described as sharp, aching or throbbing. Nociceptive pain has warning and defensive properties. The two other pain systems, neuropathic and central involve non-functional pain signals. Neuropathic pain is caused by damage to sensory nerves which send inaccurate pain messages to higher brain centers. Pain may be present despite a lack of a clear peripheral cause. 5
Clinical trials lasting from days to months involving more than 1000 patients have shown efficacy in different categories of chronic pain, but the vast majority of controlled trials have involved patients with chronic neuropathic pain. 4 “Neuropathic pain is a severe chronic, debilitating condition associated with nerve injury that develops following lesions to the central and peripheral nervous systems. Neuropathic pain often manifests as spontaneous burning, tingling, or a shooting sensation which can be amplified by noxious stimuli. 6
Recently it has been recognized that cannabinoids both endogenous and plant derived act simultaneously on multiple pain targets within the peripheral and central nervous systems. “In addition to working on CB1 and CB2 receptors, cannabinoids may reduce pain through interaction with non CB1/CB2 cannabinoid G protein coupled receptors such as GPCR 55 or GCPR18, as well as opioid or serotonin(5-HT) receptors. In addition, many studies have reported the ability of certain cannabinoids to modulate peroxisome proliferator activated receptors (PPARs), cys loop ligand gated ion channels or transient receptor potential (TRP) channels. Data suggests that there are a variety of interactions between cannabinoid, opioid and TRPV1 receptors in pain modulation. 1
Both CB1 and CB2 receptors have been found to be upregulated in nervous structures involved in pain processing in response to peripheral nerve damage.1 CB1 receptors are found at high levels in the brain but also lower levels in spinal and peripheral nervous tissue including areas important for pain perception.7 CB1 receptors are also found in brain areas involved in nociceptive perception such as the thalamus and amygdala. Data reveals that amygdala activity contributes to inter-individual responses to cannabinoid analgesia. 3 The anatomical distribution of CB1 receptors helps in identifying how these receptors function in modulating pain perception at both peripheral and central levels. 7 In addition, CB1 receptors have been shown to impede pain conduction. 8
CB2 receptors are primarily expressed in immune cells, including myeloid, macrophage, microglia, lymphoid and mast cells. 8 CB2 while commonly reported as confined to lymphoid and immune tissues, is also proving to be an important mediator for suppressing both pain and inflammatory processes. 9
There are about 100 different cannabinoids isolated from the cannabis plant. The main psychoactive compound is delta-9-tetrahydrocannabinol. It is responsible for most of the pharmacological actions of cannabis, including the psychoactive, analgesic, anti-inflammatory, anti-oxidant, antipruritic, bronchodilatory, antispasmodic and muscle relaxant activities. THC exhibits the greatest analgesic activity. 1 In fact, THC administered epidurally produces antinociception like that observed with opioid compounds. 7 THC acts as a partial agonist at CB1 and CB2 receptors. THC when acting at the CB1 receptor has been shown to modulate neural conduction of pain signals by mitigating sensitization and inflammation. 5 THC suppresses proinflammatory cytokines and enhances anti-inflammatory cytokines in both the innate and adaptive immune responses. 6 THC has twenty times the anti-inflammatory potency of aspirin and twice that of hydrocortisone. 9 In neuropathic pain cannabis containing a lower dose (1.29% THC) and higher dose (3.53% THC) delivered by vaporizer demonstrated a significant analgesic response. 6 A study using Nabilone (a synthetic THC analogue) found it to be significantly more effective than placebo in reducing pain in patients with painful diabetic neuropathy. 6 THC may have differing effects on the sensory (intensity, quality) vs affective (unpleasantness, suffering) components of pain. 3 New imaging studies show that THC works in the brain to effectively treat chronic neuropathic pain. A small trial showed that THC induced pain relief was associated with reduced functional connectivity between the anterior cingulate cortex and the sensorimotor cortex. This effect seems to involve a breakdown in functional connectivity between brain regions that process different dimensions that construct the experience of pain. 11
CBD the other major consistent of the Cannabis Sativa plant has therapeutic effects but with a different pharmacologic profile. 7 CBD has virtually no psychoactivity compared to THC. 10 The synergistic contributions of CBD to cannabis pharmacology and specifically analgesia has been scientifically demonstrated. 3 Evidence suggests that CBD alone or combined with THC can suppress chronic neuropathic pain and that CBD may have a protective effect after nerve injury.4 CBD is thought to have significant analgesic, anti-inflammatory, anti-convulsant and anxiolytic activities without the psychoactive effects of THC. CBD has little binding affinity for CB1 or CB2 receptors but is capable of antagonizing them in the presence of THC. 1 CBD regulates the perception of pain by influencing the activity of a significant number of targets (5HT1A, ion channels,TRPV1,TRPA1 ,TPRM8, GlyR, and PPARs )while also inhibiting uptake of the endogenous cannabinoid anandamide(AEA) and weakly inhibiting its hydrolysis by the enzyme fatty acid amide hydrolase(FAAH) thus enhancing the effects of anandamide. 1, 7 CBD is capable of improving the tolerability of THC by reducing THC’s psychoactive effects and antagonizing some of the other effects of THC such as tachycardia, sedation and anxiety. 1 It has low affinity for both CB1 and CB2 receptors. CBD agonist activity at CB2 receptors seems to account for its anti-inflammatory properties and both primary and secondary influences on pain. The few studies done with CBD suggest it inhibits 5-HT reuptake and there is some experimental evidence to support CBD’s activity in other neurotransmitter systems such as dopamine, GABA and the endogenous opioid system. 10 CBD along with THC inhibits glutamate neurotoxicity and displays antioxidant activity.9
It may be presumptuous to assume that the major clinical effectiveness of cannabis is derived solely from THC and CBD. In addition, non-cannabinoid constituents of the cannabis plant such as terpenes and flavonoids may contribute to the analgesic as well as anti-inflammatory effects of cannabis. 1 “The entourage effect is a term used to describe enhancement of efficacy, with related improvement in overall therapeutic effectiveness, derived from combining phytocannabinoids and other plant derived molecules. Terpenes share a precursor molecule with phytocannabinoids. Cannabis derived terpenes include limonene, myrcene, alpha-pinene, linalool, B-caryophyllene, caryophyllene oxide, nerolidol and phytol. Phytocannabinoid-terpene interactions could produce synergy with respect to treatment of pain and inflammation.” 3 Clinical data indicate that cannabinoids administered together are more effective at ameliorating neuropathic pain than the use of a single agent. 3 A controlled cannabis extract containing numerous cannabinoids and other non-cannabinoid fractions such as terpenes and flavonoids demonstrated greater antinociceptive efficacy than a single cannabinoid given alone, indicating synergistic antinoceptive interaction between cannabinoids and non-cannabinoids in a rat model of neuropathic pain. 1 Cannabis terpenoids also display numerous attributes that may be germane to pain treatment. 9
As with many analgesics’ cannabinoids do not seem to be equally effective in the treatment of all pain conditions in humans. This is probably due to the different mechanisms of pain (acute vs chronic, or chronic non-cancer vs chronic cancer pain. 1 When cannabinoids lead to a reported reduction in pain, it remains unclear where the effects are triggered or what aspect of the pain experience is most affected and under what circumstances. 4
In evaluating the indication of using cannabis for pain many of the trials involve the use of a synthetic single molecule of cannabinoid. 2 To truly evaluate cannabis’ medicinal benefit regarding pain the interplay of the various components needs further investigation as opposed to evaluating molecules in isolation.
References
1. Vučković, Sonja et al. “Cannabinoids and Pain: New Insights From Old Molecules.” Frontiers in pharmacology vol. 9 1259. 13 Nov. 2018, doi:10.3389/fphar.2018.01259
2. Deshpande A, Mallis A. Medical Cannabis and Pain Management: How Might the Role of Cannabis Be Defined in Pain Medicine? JALM Jan 2018;485-488. doi:10.1373/jalm.2017.023184
3. Fine PG, Rosenfield MJ. Cannabinoids for Neuropathic Pain. Curr Pain Headache Rep 2014; 18:451-459. doi:10.1007/s11916-014-0451-2.
4. Fine PG, Rosenfield MJ. The Endocannabinoid System, Cannabinoids, and Pain. Rambam Maimonides Med J. 2013;4(4). doi:10.5401/RMMJ.10129
5. Hill KP, Palastro MD, Johnson B, Ditre JW. Cannabis and Pain: A Clinical Review. Cannabis and Cannabinoid Research 2017;(2):96-104 http://online.liebertpub.com/ doi:10.1089/can.2017.0017
6. Donvito G, Nass SR, Wilkerson JL, Curry ZA, Schurman LD, Kinsey SG, Lichtman AH. The endogenous Cannabinoid System: A Budding Source of Targets for Treating Inflammatory and Neuropathic Pain. Neuropsychopharmacology Reviews 2018; 43:52-79. doi:10.1038/npp2017.204.
7. Manzanares, J et al. “Role of the cannabinoid system in pain control and therapeutic implications for the management of acute and chronic pain episodes.” Current neuropharmacology vol. 4,3 (2006): 239-57. doi:10.2174/157015906778019527
8. Modesto-Lowe V, Bojka R, Alvardo C. Cannabis for peripheral Neuropathy: The good, the bad, and the unknown. Cleveland Clinic Journal of Medicine.85(12):943-949. Doi.10.3949/ccjm.85a.17115.
9. Russo E. Cannabinoids in the management of difficult to treat pain. Therapeutics and Clinical Risk Management 2008;4(1):245-259. Accessed November 24, 2019.
10. Russon EB, Burnett A, Hall B, Parker KK. Agonistic Properties of Cannabidiol at 5-HT1a Receptors. Neurochemical Research;30(8):1037-1043. Doi:10.1007/s11064-005.6978-1
11. McNamara D. Cannabis for Chronic Nerve Pain: Mechanism Revealed? https://www.medscape.com/viewarticle/901689 September 7, 2018 Accessed November 24, 2019.

Cannabidiol (CBD) and tetrahydrocannabinol (THC) are both naturally occurring compounds found in Cannabis. Delta-9-tetrahydrocannabinol (∆9-THC) was the first cannabinoid to be discovered and studied and is well known for its psychoactive effects. 2 Cannabidiol (CBD), like ∆9-THC is a major phytocannabinoid and is non-psychotropic.3 The endocannabinoid system (ECS) consists of two types of endogenous G-protein coupled cannabinoid receptors, CB1 and CB2. The CB1 receptor is located primarily in the central and peripheral nervous system and found abundantly in the brain. CB2 receptors are distributed widely in the tissues of the immune system. 3 Obesity is a major public health concern increasing the risk of diabetes, cancer, and cardiovascular disease. Worldwide nearly 1.9 billion adults are overweight and 600 million are obese. 4 The development of obesity involves a complex interaction between genetics, diet, and environmental factors but there are differences in the bacterial composition of the microbiome in individuals who are overweight or obese. The microbiome is the genetic material of all the microbes including bacteria, fungi, protozoa, and viruses that live on and inside the human body(microbiota).5 The majority live in our gut, particularly in the large intestine. The gut microbiota can alter host body weight and plays a role in the development of diet-induced obesity. Several studies are looking at alterations in the microbiome leading to obesity. 6 “It is well established that the endocannabinoid system is involved in both the regulation of energy balance and the development of obesity. Gut microbiota regulates adipogenesis through endocannabinoid signaling”. 7 The endocannabinoid system interacts with several neuropeptides that modulate hunger and satiety including ghrelin 8 and leptin. 4 Leptin reduces food intake by upregulating anorexigenic (appetite-reducing) neuropeptides and ghrelin is a potent orexigenic (appetite-stimulating) brain-gut peptide with lipogenic and diabetogenic effects 4,8 Microbial DNA sequencing has demonstrated that the mammalian gut microbiota is predominantly composed of four bacterial phyla: Gram-negative Bacteroidetes and Proteobacteria and Gram-positive Actinobacteria and Firmicutes. Studies investigating the possible relationship between gut microbiota composition and obesity were in a leptin-deficient ob/ob mouse model. This model revealed a reduction in the abundance of Bacteroidetes and a proportional increase in Firmicutes.9 A study conducted by Ley et al. 10 observed analogous differences in the distal gut microbiota in human obesity. The authors suggest that Firmicutes produce more complete metabolism of a given energy source than do Bacteroidetes, promoting more efficient absorption of calories and subsequent weight gain. In a recent study chronic administration of THC prevented weight gain in diet-induced obesity in mice and the investigators suggest that these actions may be mediated in part by modifications of the gut microbiota. The same study found that in diet-induced obesity in mice chronic THC administration increased Akkermansia mucinphilia levels. Akkermansia mucinphilia has been shown to regulate fat storage and adipose tissue metabolism leading to weight loss. 7 “Traditionally, adipose tissues have been divided into subcategories of white adipose tissue (WAT) and brown adipose tissue (BAT) according to their function and morphology. Brown adipose tissue is characterized by small lipid droplets and a high density of mitochondria which leads to the brown appearance. White adipose tissue stores and releases fatty acids and these fatty acids are stored in a large unilocular lipid droplet giving it a white appearance. Brown adipose tissue is involved in thermogenesis and caloric expenditure during rest and exercise”. 11 White adipose tissue is involved in fat storage and endocrine secretion of hormones. In response to various types of stimuli white adipose tissue can become beige adipose tissue (browning of white fat,). “Recruitment of the brown-like phenotype in white adipocytes and activation of existing brown adipocytes are currently being investigated as a potential treatment for obesity and recent studies suggest that CBD may play a role in the browning of adipocytes and thus may be a potentially promising therapeutic agent in the prevention of obesity.”12 There is a research gap that exists in studies investigating CBD’s effect on food intake, food preferences, and weight gain in rats which have shown contradictory results some demonstrate CBD induced a decrease in weight gain while other studies have shown no significant impact on food intake or body weight in mice and rats. 13 References 1. Rudd, J. CBD vs THC-What are the Main Differences? https://www.analyticalcannabis.com/articles/cbd-vs-thc-what-are-the-main-differences-297486. Published Feb 20, 2018. Accessed March 21, 2021. 2. Pisanti, S et al. Cannabidiol: State of the art and new challenges for therapeutic applications. Pharmacology & Therapeutics 2017.http://dx.doi.org/10.1016/j.pharmthera.2017.02.041 3. Maroon J, Bost J. Review of the neurological benefits of phytocannabinoids. Surg Neurol Int. 2018;9:91. Published 2018 Apr 26. doi:10.4103/sni.sni_45_18 4. Rossi F, Punzo F, Umano GR, Argenziano M, Miraglia Del Giudice E. Role of Cannabinoids in Obesity. Int J Mol Sci. 2018 Sep 10;19(9):2690. doi: 10.3390/ijms19092690. PMID: 30201891; PMCID: PMC6163475. 5. Ferranti EP, Dunbar SB, Dunlop AL, Corwin EJ. 20 things you didn't know about the human gut microbiome. J Cardiovasc Nurs. 2014;29(6):479-481. doi:10.1097/JCN.0000000000000166 6. Castaner O, Goday A, Park YM, et al. The Gut Microbiome Profile in Obesity: A Systematic Review. Int J Endocrinol. 2018;2018:4095789. Published 2018 Mar 22. doi:10.1155/2018/4095789 7. Cluny NL, Keenan CM, Reimer RA, Le Foll B, Sharkey KA. Prevention of Diet-Induced Obesity Effects on Body Weight and Gut Microbiota in Mice Treated Chronically with Δ9-Tetrahydrocannabinol. PLoS One. 2015 Dec 3;10(12):e0144270. doi: 10.1371/journal.pone.0144270. PMID: 26633823; PMCID: PMC4669115. 8. Lim CT, Kola B, Feltrin D, et al. Ghrelin and cannabinoids require the ghrelin receptor to affect cellular energy metabolism. Mol Cell Endocrinol. 2013;365(2):303-308. doi:10.1016/j.mce.2012.11.007 9. Clarke SF, Murphy EF, Nilaweera K, Ross PR, Shanahan F, O'Toole PW, Cotter PD. The gut microbiota and its relationship to diet and obesity: new insights. Gut Microbes. 2012 May-Jun;3(3):186-202. doi: 10.4161/gmic.20168. Epub 2012 May 1. PMID: 22572830; PMCID: PMC3427212. 10. Ley, R., Turnbaugh, P., Klein, S. et al. Human gut microbes associated with obesity. Nature 444, 1022–1023 (2006). https://doi.org/10.1038/4441022a 11. Kaisanlahti A, Glumoff T. Browning of white fat: agents and implications for beige adipose tissue to type 2 diabetes. J Physiol Biochem. 2019;75(1):1-10. doi:10.1007/s13105-018-0658-5 12. Parray HA, Yun JW. Cannabidiol promotes browning in 3T3-L1 adipocytes. Mol Cell Biochem. 2016 May;416(1-2):131-9. doi: 10.1007/s11010-016-2702-5. Epub 2016 Apr 11. PMID: 27067870. 13. Bielawiec P, Harasim-Symbor E, Chabowski A. Phytocannabinoids: Useful Drugs for the Treatment of Obesity? Special Focus on Cannabidiol. Front Endocrinol (Lausanne). 2020;11:114. Published 2020 Mar 4. doi:10.3389/fendo.2020.00114

The transmucosal route of delivery occurs when drugs diffuse through a mucous membrane. The oral cavity can be utilized for transmucosal delivery and the challenge of limited surface area and salivary action can be overcome with efficient agents and appropriate administration.1 Transmucosal delivery methods include dissoluble films, tinctures, oral sprays, and lozenges and target the buccal and sublingual areas. “Sublingual and buccal formulations depend on the efficient transfer of a drug from a hydrophilic vehicle to the cell membranes of the sublingual or buccal mucosa. The buccal and sublingual mucosa have venous drainage directly into the vena cava and the left side of the heart. Substances absorbed through the mucosa of these areas avoid the liver and the subsequent hepatic first-pass effect. The avoidance of the first pass effect is the rationale for the use of the transmucosal mode of delivery. Drug transport across the mucosa can be trans or paracellular. Absorption of cannabinoids likely takes place through the interstices in the membrane or by transfer into the epithelial cells.”2 When developing agents for this route of administration the formulation requires the use of mucoadhesive agents to maintain an intimate and prolonged contact of the formulation with the absorption site, penetration enhancers, to improve drug permeation across the mucosa, enzyme inhibitors to protect the drug from degradation through mucosal enzymes and solubility modifiers to enhance the solubility of poorly soluble drugs.3 The sublingual mucosa is more permeable, vascularized, and thinner than the buccal mucosa. The sublingual route of administration of cannabinoids has a rate of absorption intermediate between that achieved by smoking and the oral route. 2.This absorption delay provides patients with the ability to titrate their dose to exploit the window between wanted therapeutic effects and unwanted side effects.2 Saliva is a water-rich environment with a mucus component. Salivary flow determines the amount of time a drug spends in the oral cavity. Salvia production can cause difficulties in maintaining contact between the dosage form and the sublingual mucosa. This can result in short exposure times and unpredictable distribution of the drug on the site of action/absorption.3 Sublingual formulations may stimulate the flow of saliva making it difficult for patients not to swallow the medication. If cannabinoid medications applied to the sublingual mucosa are swallowed the cannabinoids will be subject to the first-pass effect and will be less effective and result in the production of metabolites. 2 Buccal formulations where the product is held in contact with the parietal buccal membrane may be subject to the same limitations. 2 The buccal area is the inner lining of the cheek and the lip and encompasses about one-third of the surface area of the oral cavity. 3,4The buccal mucosa consists of a surface layer of stratified epithelium linked to underlying connective tissue. There is a network of blood capillaries in the connective tissue where drugs that have permeated through the epithelium can enter the systemic circulation.1,4 The buccal membrane has lower permeability when compared to the sublingual membrane. 2,3, The absorption potential of the buccal mucosa is influenced by the lipid solubility and molecular weight of the diffusant. Solubilization of poorly water-soluble drugs by complexation with cyclodextrins is advantageous in increasing drug absorption and bioavailability via the buccal mucosa.3 When formulating a buccal medication there is a need for penetration enhancers.2,4 Penetration enhancers are substances that help open intercellular tight junctions. Permeation/penetration enhancers work by different mechanisms including changing mucus rheology, increasing the fluidity of the lipid bilayer membrane, acting on tight junctions, overcoming enzymatic activity, and increasing thermodynamic activity. These mechanisms result in better drug absorption. Examples of penetration enhancers include sodium lauryl sulfate, oleic acid, cyclodextrin, and chitosan. 2 The improper selection or use of these enhancers can cause tissue irritation The turnover of the buccal epithelium is about three to eight days and this rapid turnover can reduce the risk of tissue damage or irritation. Another concern when using these enhancers is an undesired bolus effect which may lead to an increase in the concentration of the drug in the blood to levels that may not be safe. 4Additional factors influencing the absorption of a drug through the buccal mucosa include when and what the patient eats, drinks, or smokes and the location where the patient places the dosage. 4 Mucoadhesive films are a preferred dosage form for buccal mucosa administration. Mucoadhesive films stay in contact with the mucosa longer, cover a larger surface area, and can provide more accurate drug dosing. Film composition is designed to achieve bioadhesive strength, tensile strength, pliability, flexibility, and extended disintegration. Achieving this is highly dependent on the type and concentration of the selected polymers and the dose of active ingredients being delivered.4 Film formulations include polymers, permeation enhancers, and lipids which are combined to optimize drug diffusion and permeation through the mucosa.4 There is a method of transmucosal delivery of cannabinoids via a film matrix utilizing hot-melt extrusion, hot melt molding, admixing, or solvent cast techniques. 5 Additional routes of oromucosal delivery include lozenges and tinctures. Lozenges can be solid, soft, or chewable. Cannabinoids are usually formulated in soft or chewable forms. 6 Typically a solid lozenge dissolves and coats the oral cavity and the top one-third of the esophagus. Solid dose forms display greater inter and intraindividual variations in absorption and bioavailability. The dissolution rate of a lozenge depends on how hard the patient sucks on the lozenge and saliva production. It takes roughly 30 minutes for a lozenge to dissolve and this short time frame limits how much drug can be delivered. 1 Tinctures are a classical method of plant-based delivery and have been used for centuries to prepare cannabis medicines. Tinctures are best taken sublingually. Cannabis can be delivered in a rapid, dose measured manner as a tincture. Tinctures are extracts of cannabis in an organic solvent, such as alcohol or glycerin. When alcohol-based products like tinctures are used the alcohol acts as a delivery method and circumvents the digestive tract so it is absorbed directly into the bloodstream. as a result, tinctures are fast-acting. 7 Much of our knowledge of cannabinoid absorption via the oromucosal route comes from studies done on Sativex, a whole plant cannabis extract. Sativex (Nabximols) contains nearly equivalent THC and CBD concentrations and is delivered via spray onto the oral mucosa to improve bioavailability. Following administration of Sativex both THC and CBD are absorbed rapidly. When Sativex is administered oromucosally, plasma levels of THC and other cannabinoids are lower compared with the levels achieved following inhalation of cannabinoids at a similar dose. Researchers believe these differences are due to slower absorption and redistribution of the cannabinoids into fatty tissues. Additionally, some of the THC undergoes hepatic first-pass metabolism to 11-OH-THC and some of the CBD is metabolized to 7-OH-CBD. 8 References 1. Sapanaro DM,Winberg MA. Transmucosal Drug Delivery in the Oral Cavity. https://decisionsindentistry.com/article/transmucosal-drug-delivery-in-the-oral-cavity/. Published Dec 12, 2018. Accessed April 20, 2020. 2. Whittle BA, Guy GW, Robson P. Prospects for New Cannabis Based Prescription Medicine. http://www.cannabis-med.org/iacm/data/pdf/2001-03-04-11.pdf. Accessed April 6, 2020. 3. Reddy PC, Chaitanya KS, Rao YM. A Review on bioadhesive buccal drug delivery systems: Current status of formulation and evaluation methods. DARU Journal of Pharmaceutical Sciences. 2011;19(6):385-403. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3436075/ Accessed April 20, 2020. 4. Buccal Films- Better Drug Release & Patient Experience With Buccal Films. https://drug-dev.com/buccal-films-better-drug-release-patient-experiences-with-buccal-films/ Accessed April 20, 2020. 5. Eloshly M, Repka M, inventors; University of Mississippi, assignee. Transmucosal delivery of cannabinoids. United States patent application US 10/516,188. 2006 Nov. 16. https:// patioentimages.storage.googleapis.com/d5/39/4a/56cdf49477be06/US20060257463A1.pdf Accessed April 202,2020. 6. Pearson R. MCST603 Module 6 Lecture 4. Accessed April 20, 2020. 7. Nazarenus C. Medical Cannabis Handbook For Healthcare Professionals. New York, New York: Springer Publishing Company;2020 8. Sativex Oromucosal Spray 5.2 Pharmokinetic properties. http://www.medicines.org/uk/emc/medicine/23262 Accessed April 20, 2020.

The burgeoning interest in the therapeutic potential of cannabis has brought to the fore the complexities of its various chemovars and their interactions with the human endocannabinoid system. As a plant with a rich pharmacological tapestry, cannabis contains a multitude of compounds, each with distinct effects on the body. The term "chemovar," a portmanteau of "chemical" and "cultivar," refers to the specific chemical profile of a cannabis plant, which can significantly influence its therapeutic properties. Concurrently, the endocannabinoid system, a network of receptors and neurotransmitters, plays a crucial role in maintaining human homeostasis, affecting functions such as mood, appetite, and pain sensation. The intricate dance between these chemovars and the endocannabinoid system suggests a nuanced potential for personalized medicine, yet it also presents a challenge for researchers and clinicians seeking to optimize therapeutic outcomes. The crux of this exploration lies in the hypothesis that specific cannabis chemovars exert differential effects on the endocannabinoid system, thereby modulating physiological responses in a manner that could be tailored to individual needs. Different cannabis chemovars along with their pharmacological profiles, and the mechanisms by which they interact with the endocannabinoid system provide the potential for targeted therapeutic strategies, and a deeper understanding of these interactions will not only advance our knowledge of cannabis as a complex botanical medicine but also enhance our ability to harness its properties for the benefit of diverse patient populations.

The DSM-5 now recognizes a cannabis related disorders category that includes cannabis use disorder (CUD), cannabis intoxication, cannabis withdrawal, other cannabis-induced disorders, and unspecified cannabis related disorder.1 Chronic cannabis use is associated with an increased risk of developing cannabis use disorder. 2 In the DSM-5 cannabis use disorder includes 11 criteria which are like other substance use disorders and they encompass the range of signs and symptoms including physiological signs like tolerance and withdrawal. 3 The DSM-5 defines cannabis dependence as a disorder characterized by a problematic pattern of use leading to clinically significant impairment or distress. Approximately 10% of individuals who regularly use cannabis will develop dependence. In the DSM-5 cannabis abuse and dependence fall under the diagnosis of CUD. 4 Clinical and experimental work spanning the last two decades has indicated that cannabis specifically THC has the potential to be abused. 3 Cannabis has been associated with low abuse potential compared to other drugs of abuse, but it would be inappropriate to underestimate its abuse and dependence liability. Cannabis addiction has been observed in about 9% of users. 5 In human studies of abuse potential, cannabis produces clear subjective reports of pleasurable effects, and these are associated with motivational responses including drug-seeking and drug-taking behavior. Euphoria or a feeling of being high has been identified as a primary factor associated with cannabis use.6 Many factors contribute to the abuse liability of cannabis but one that must be considered is that THC potency has increased steadily over the last four decades. 1 Chronic cannabis users typically experience unpleasant withdrawal symptoms when use is discontinued. Cannabis withdrawal symptoms include restlessness, irritability, and insomnia just to name a few.2,5 Symptoms of cannabis withdrawal also seem to appear in a similar time course and manner as withdrawal from other substances of abuse. These symptoms are much less severe than those associated with withdrawal from opioids but aversive enough to encourage continued cannabis use and interfere with cessation attempts. 1 Whether a drug can influence the dopaminergic system aids in determining if a drug could possess abuse potential through its reinforcing actions. Increased dopamine release in cells of the mesolimbic ventral tegmental area and the nucleus accumbens pathway is a common characteristic of almost all drugs of abuse and THC has been shown to increase dopamine in these areas. ,6 Research indicates that there are interactions between dopamine receptors(D2) and CB1 receptors.5 Although cannabis may have lower abuse liability than other drugs like cocaine or nicotine, once somebody develops dependence quitting becomes extremely difficult. Relapse rates observed for cannabis use disorders are comparable to those for other abused drugs and only 15-37% of patients undergoing psychotherapeutic and pharmacological interventions achieve continued abstinence.1,3 Many individuals use cannabis for its psychoactive effects When drug-associated cues and contexts associated with the initial exposure to a drug are highly rewarding a conditioned dopamine release can occur. 2 Through the process of conditioning and learning these specific cues in the environment gain control of behavior. This activates and guides a complex sequence of actions required to obtain, prepare, and self-administer the drug, and over time this behavior can become increasingly habitual and resistant to change even after a long period of abstinence. 1 References 1. Panlilio, L V et al. “Cannabinoid abuse and addiction: Clinical and preclinical findings.” Clinical pharmacology and therapeutics vol. 97,6 (2015): 616-27. doi:10.1002/cpt.118 2. Zehra, Amna et al. “Cannabis Addiction and the Brain: A Review.” Journal of neuroimmune pharmacology : the official journal of the Society on NeuroImmune Pharmacology vol. 13,4 (2018): 438-452. doi:10.1007/s11481-018-9782-9 3. Piomelli D, Haney M, Budney AJ, Piazza PV. Legal or Illegal, Cannabis Is Still Addictive. Cannabis and Cannabinoid Research 2016; 1: 47-53. https://www.liebertpub.com/doi/pdf/10.1089/can.2015.29004.rtd 4. Siavash J, Tan T. Diagnosis and Treatment of Marijuana Dependence. British Columbia Medical Journal 2016;58(6):315.317. https://www.bcmj.org/articles/diagnosis-and-treatment-marijuana-dependence Accessed June 11, 2020. 5. Jain R, Pal Y, Balhara. Neurobiology of Cannabis Addiction Indian J.Physiol Pharacol 2008;52(3):217-232 https://pdfs.semanticscholar.org/73ec/29608ca979e9ff1423d3e0ed4b4e19ba06ba.pdf Accessed June 11, 2020. 6. White J. Abuse and dependence potential of Cannabis sativa and nabiximols. 2016; 38th ECDD Agenda item 5.1 https://www.who.int/medicines/access/controlled-substances/Abuse_and_dependence_potential.pdf?ua=1 Accessed June 11, 2020.

Kandel and Faust in the 1970s conducted a study with secondary students in New York State where they described a sequence of substance use initiation progressing from alcohol use to tobacco use followed by cannabis and then other substance use. The authors initially cautioned that their findings should not be considered casual but suggested later that some substances are a gateway to others. this became known as the “gateway hypothesis”. 1 The term “gateway drug” was popularized in 1984 by Dr. Robert L. DuPont Jr. who posited that if young people did not use cannabis it was relatively unlikely that they will use other illegal drugs, He did not claim that cannabis use causes young people to use other drugs. Dr. DuPont observed that if young people did not use alcohol or tobacco, they would be less likely to use other drugs such as cannabis. His main conclusion was that a young person’s willingness to use any drug and especially frequent use may remove the psychological barrier to using another drug. 2 Research does not support the theory that cannabis is a “gateway drug”. Cannabis has never been proven to have a gateway effect. 1,2 Association does not prove causation. 2 Individuals who have used drugs such as heroin or cocaine are more likely to have used cannabis than someone who has not used any of these substances. Since cannabis is the most widely obtainable and widely used illicit drug individuals are more likely to have used cannabis before other illicit drugs as a result. If the gateway effect were true, more cannabis users would progress in their drug use which is not the case. The vast majority of people who use cannabis do not go on to use other illicit drugs. 2 Cannabis use may be associated with other substances, but it involves complex relationships with other factors such as adverse childhood experiences, social influences, genetic, environmental factors, and mental health issues. 1 Research suggests that those who use drugs may have an underlying propensity to do so that is not specific to any drug. 2 Most drug users typically begin with underage nicotine and alcohol use before cannabis. 3 Some suggest that adolescents who have a propensity for drug use are exposed to other drugs when purchasing cannabis on the black market which then increases the opportunity to use other illicit drugs. 4 It is important to recognize that most of the research on drug progression has focused on recreational use. Research from states with medical marijuana programs has found that youth rates drop or remain stable after a state passes a medical marijuana law. A study conducted 15 years after the passage of the first medical marijuana law concluded that teens’ cannabis use has generally decreased. 2 References 1. Leece P, Paul N. Q&A:Is cannabis a “gateway drug? Ontario Agency for Health and Promotion(Public Health Ontario) Toronto,ON:Queen’s Printer for Ontario; Published 2019. https://www.publichealthontario.ca/-/media/documents/Q/2019/qa-cannabis-gateway.pdf?la=en Accessed September 26, 2020. 2. Alexander C. Debunking the “Gateway” Myth. Drug Policy Alliance. Published February 2017. https://www.drugpolicy.org/sites/default/files/DebunkingGatewayMyth_NY_0.pdf Accessed September 26, 2020. 3. Scharff C. Marijuana:The Gateway Drug Myth. Psychology Today. Posted Aug 26, 2014. https://www.psychologytoday.com/us/blog/ending-addiction-good/201408/marijuana-the-gateway-drug-myth Accessed September 26, 2020 4. Jaffe A. Is Marijuna a Gateway Drug? Psychology Today .Posted Jul 24, 2018. https://www.psychologytoday.com/us/blog/all-about-addiction/201807/is-marijuana-gateway-drug Accessed September 26, 2020.
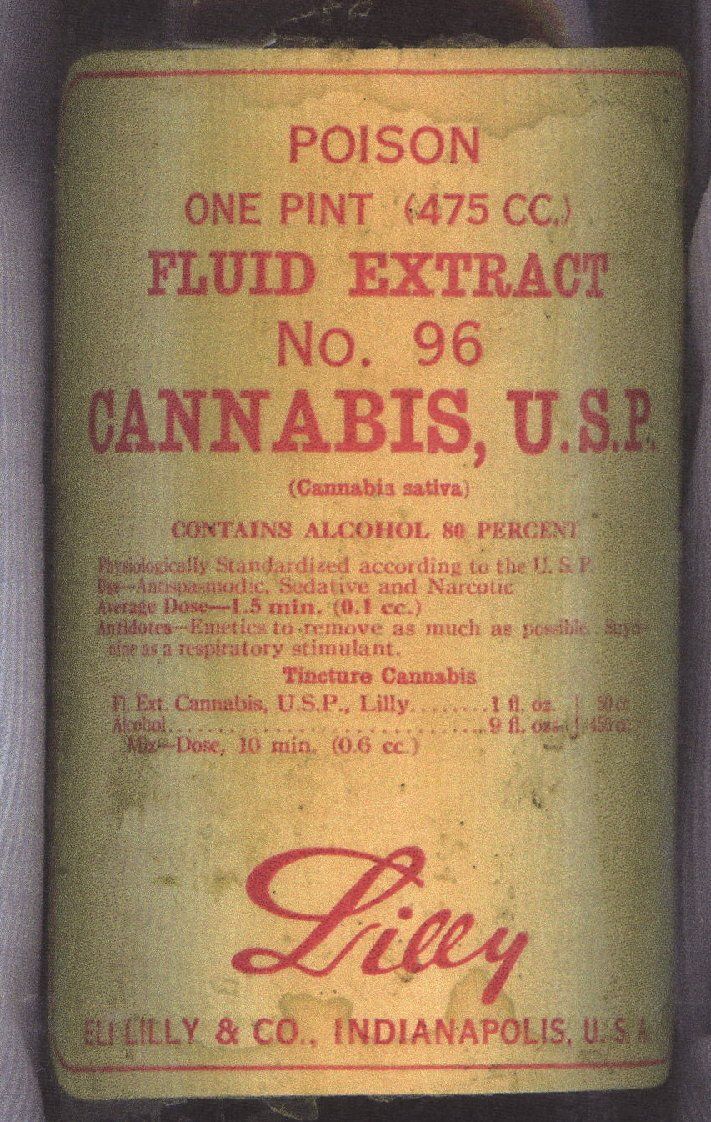
There is a need for USP standards for cannabis to be accepted by the medical community it must conform to the same standards and regulations as any other medicine. Cannabis must be tested so patients know what they are using, providers know what to recommend, and product labels need to be accurate. Currently, there is no federal oversight or regulatory control, instead, the laws governing the testing of cannabis have been left up to the states. Some states have very stringent controls in place while others do not, which has put the consumer at risk. Consumers and patients expect quality to be inherent in the products they use, and poor-quality control procedures can lead to adverse events and increased health risks. These standards could also provide access to quality materials for use in clinical trials. These trials are needed to demonstrate the safety and efficacy of cannabis.1 The United States Pharmacopeia (USP) is a scientific nonprofit organization that plays a role in developing and formulating standards for medicines, dietary supplements, and foods based on expert advice from the medical and scientific community. 1 Once the USP determines there is a need for guidance, methodology, or standards for a new industry, product, or process they produce a draft standard and guidance document. Once the draft is approved the monographs, chapters, and other standards are published in the Unites States Pharmacopeia-National Formulary (USP-NF). 2 Monographs are documents that explain the expectations for a food, drug, or material to ensure its identity, purity, strength, and performance. Monographs contain the chemical information for the ingredient or material and outline the tests and procedures that must occur to meet quality criteria and limit impurities. General chapters provide information on accepted processes, tests, and methods to support industry in product development and manufacturing quality controls. General chapters must be referenced in a specific monograph to be enforceable on a legal basis. 2 The 1938 Food Drug and Cosmetic Act decreed that all medicines sold in the United States must meet USP quality standards. USP standards are enforced by the FDA. Since cannabis is a Schedule 1 drug and is illegal at the federal level, USP has not created a formal official compendium. 2,3 Cannabis first appeared in the 1850 edition of the United States Pharmacopoeia and the Extractum Cannabis monograph was published. In 1916, USP published the Cannabis americana monograph. In 1936 USP published an additional monograph, USP XI. Cannabis was removed from the pharmacopeia in 1940.3 With the reemergence of cannabis as a medicinal product, the goal of the USP is to ensure the quality of cannabis intended for medical purposes. It is imperative for public safety that the USP develop standards to address laboratory verification of cannabis identity, quantitative analysis of cannabinoids and terpenes, and measures to limit exposure to contaminants such as mycotoxins, pesticides, and heavy metals.2 One of the first challenges the USP had to address was how to classify the various varieties and subtypes of the plant product. USP has divided the plant material into three main chemotypes based on the amount of THC and CBD present. These three classifications are, THC dominant, CBD dominant, or intermediate containing both THC and CBD. 1,2This classification system is needed since brand names associated with strain names such as Sativa or Indica can be misleading. 1There can be considerable variation in cannabinoid content among specimens of the same strain and the total THC and CBD levels of a given chemotype can be profoundly affected by cultivation methods, processing, and storage conditions. These factors can be altered to produce strains with higher THC levels.3 USP recommends the use of science-based analytical procedures to identify cannabis varieties. These techniques include high-performance liquid chromatography (HPLC) and gas chromatography (GC) to separate and quantify THC, CBD, and 11 other cannabinoids that may have therapeutic potential.1,3 Reference materials or physical standards currently produced by USP can be used to confirm the identity of various cannabinoids by chromatographic techniques. 1,2 Different cannabis varieties can also vary in the composition of terpenes. USP identified five different terpenes that are abundant in cannabis and recommends profiling these terpenes via separate GC procedures. These detailed profiles of cannabinoid and terpene content can help guide prescribers and ensure patients that they are receiving a consistent product.1 USP standards establish guidelines to ensure safety and create analytical limits for possible contamination from pesticides, heavy metals, mycotoxins such as aflatoxin, and adulteration. One of the most cited reasons for the recall of cannabis products was the contamination of products with pesticides due to exceeding state limits or the presence of restricted pesticides.2 Since cannabis is classified as a schedule one drug, there are no federally approved crop protection agents, this is regulated at the state level. With the absence of legal guidance, growers have used pesticides not intended for use with food or medicinal crops. The US Environmental Protection Agency regulates pesticides for food crops but there is no specific tolerance or exemption for cannabis. 1 The USP maximum acceptable exposure limits for each pesticide are 1000-fold lower than the acceptable daily intake established by the Food and Agriculture Organization of the United Nations and the World Health Organization. Also, the nature and extent of risk could differ for a smoked or vaporized product compared to dietary exposure. USP general chapter articles of botanical origin establish pesticide limits based on acceptable daily exposure, body weight consumed, and a safety margin for oral exposure that can be used for the development of pesticide residue standards for inhaled cannabis materials. Cannabis is a concentrator of heavy metals which then accumulate in the plant and pose a health risk. There have been several product recalls that have occurred due to elevated levels of heavy metals 2Potential sources of elemental impurities include environmental pollutants, manufacturing, processing, and delivery sources. There are no federal testing requirements for heavy metals but rather is regulated at the state level. Most states test for four metals, cadmium, arsenic, lead, and mercury but this is not sufficient. There is a need for a federally regulated list of possible elemental containments that should be tested, instead of the patchwork of testing that currently exists at the state level. USP has several chapters on heavy metal limits and testing, which could be applied to cannabis. 2,4 Cannabis plants are susceptible to microbial contamination including molds especially Aspergillus fumigatus and mycotoxins such as aflatoxins during cultivation, harvesting, drying, storage, and/or distribution. Aspergillus spores can survive when cannabis is smoked or vaporized and can subsequently infiltrate the lungs causing infections resulting in respiratory injury which may be fatal for patients with a weakened immune system. Currently, there is no validated test for Aspergillus. There are USP chapters that address standards for monitoring microorganisms and aflatoxins which can be applied to create limits and methodologies for cannabis.1,3 There is also a need for quality standards for medical cannabis that ensures the identity purity and strength of cannabis to reduce the possibility of adulteration. Cannabis has been mixed with synthetic analogs to increase its psychotropic effect. USP has recently addressed this issue with the development of a new general chapter, Adulteration of Dietary Supplements with Drug and Drug Analogs. This approach could be used to develop cannabis standards to detect this type of adulteration. 3 There is also a need to establish guidelines addressing the potential exposure to toxic solvents used to prepare cannabis extracts. Exposure to these solvents poses a significant health risk. USP has developed procedures and general approaches described in the general chapter Residual Solvents that could be applied to address this risk in cannabis products.1,3 Without the availability of references standards produced by the USP it would be difficult to ensure that products available to a consumer are of the appropriate identity, strength, quality, purity or consistency. These standards are used in pharmaceutical development and manufacturing. To ensure that references materials produced by USP meet the highest standards they are evaluated by multiple independent laboratories. 5 Reference standards help to confirm accuracy and reproducibility in testing, they are required so analytical procedures accurately identify and measure the content of constituents in a material. Reference standards may also be used for qualitative applications such as identification tests, system suitability tests, or chromatographic peak markers. 6 The USP produces cannabis reference standards for medicinal cannabis which provide for the consistent characterization of cannabis for medical use. These references standards are used in analytical procedures to verify the identity and determine the constituents of product samples. The USP has developed multiple compounds including USP Delta-Tetrahydrocannabinol 1 mL (l mg/mL), USP Exo-Tetrahydrocannabinol 1 mL, USP cannabinoid Acid Mixture 1 mL (in acetonitrile and triethylamine with stabilizer, USP Cannabinoids Mixture 1 mL (in methanol), USP Cannabidiol Solution 1mL (lmg.ml) and USP Cannabidiol 25 mg. These reference standards can be used for the quantitative measurement of cannabinoids which is vital in the determination of potency. 7 References 1. Eisenstein M, Muldoon Jacobs KL. Cannabis for Medical Use: Consistent Quality to Help Protect Patients. USP. https://cdn2.hubspot.net/hubfs/3402974/USP%20%7C%20Cannabis%20for%20medical%20use%20consistent%20quality%20to%20help%20protect%20patients.pdf Accessed November 12, 2020. 2. Atkins PL. Everything Old is New Again: Cannabis Returns to USP. Cannabis Science and Technology. June 2020;3(5):17-22 https://www.cannabissciencetech.com/view/everything-old-new-again-cannabis-returns-usp 3. Giancaspro GI, Kim NC, Venerna J, et al. The Advisability and Feasibility of Developing USP Standards for Medical Cannabis. In Pharmacopeial Forum 2016;42(1). https://www.uspnf.com/sites/default/files/usp_pdf/EN/USPNF/usp-nf-notices/usp_stim_article_medical_cannabis.pdf Accessed November 12, 2020. 4. Thomas BF, ElSohly MA. Chapter 4: Analytical Methods in Formulation Development and Manufacturing. Thomas BF, ElSohly MA, eds. The Analytical Chemistry of Cannabis: Quality Assessment, Assurance, and Regulation of Medicinal Marijuana and Cannabinoid Preparations. Elsevier; 2015:63-82. 5. USP Reference Standards. https://www.usp.org/reference-standards Accessed November 14, 2020 6. Sarma, ND, et al, Cannabis Inflorescence for Medical Purposes: USP Considerations for Quality Attributes. Journal of Natural Products. 2020; 83(4):1334-1351 https://dx.doi.org/10.1021/acs.jnatprod.9b01200 7. Cannabis References Standards https://www.usp.org/dietary-supplements-herbal-medicines/cannabis Accessed November 14, 2020.

Terpenes are organic compounds that are produced by a variety of plants. When terpenes are modified chemically through oxidation or structural rearrangement the resultant compounds are called terpenoids. The term terpene is used to include all terpenoids. The difference between terpenes and terpenoids is that terpenes are hydrocarbons but terpenoids contain additional functional groups such as oxygen moieties or branching methyl groups. More than 200 terpenoids have been identified in cannabis. Terpenoids are pharmacologically active due to their lipophilic nature which enables interaction with cell membranes, neuronal and muscle ion channels, neurotransmitter receptors, G-protein coupled receptors and enzymes. Terpenoids are bioavailable in high percentages due to their lipophilic properties, permitting passive migration across biological membranes. Some of the most common terpenes in cannabis are D-limonene, B-myrcene, Alpha-pinene, D-linalool and Beta-caryophyllene”. 1. When terpenes work with cannabinoids like CBD and THC, they form a synergy. The entourage effect is the term used to describe this biological synergy between cannabinoids and other compounds such as terpenes. which causes enhanced effects than either would achieve on their own, one such effect that is seen is the improvement in the absorption of cannabinoids. 2 It may be presumptuous to assume that the major clinical effectiveness of cannabis is derived solely from THC and CBD. Non-cannabinoid constituents of the cannabis plant such as terpenes and flavonoids may contribute to the analgesic as well as anti-inflammatory effects of cannabis. 3 “The entourage effect is a term used to describe enhancement of efficacy, with related improvement in overall therapeutic effectiveness, derived from combining phytocannabinoids and other plant derived molecules. Terpenes share a precursor molecule with phytocannabinoids. Cannabis derived terpenes include limonene, myrcene, alpha-pinene, linalool, B-caryophyllene, caryophyllene oxide, nerolidol and phytol. Phytocannabinoid-terpene interactions could produce synergy with respect to treatment of pain and inflammation.” 4 Clinical data indicate that cannabinoids administered together are more effective at ameliorating neuropathic pain than the use of a single agent. 4 A controlled cannabis extract containing numerous cannabinoids and other non-cannabinoid fractions such as terpenes and flavonoids demonstrated greater antinociceptive efficacy than a single cannabinoid given alone, indicating synergistic antinoceptive interaction between cannabinoids and non-cannabinoids in a rat model of neuropathic pain. 3 Cannabis terpenoids also display numerous attributes that may be germane to pain treatment. 5 1. Nahitigal I, Blake A, Hand A, Florentius-Mefailoski AF, Hashemi H, Friedberg J. The Pharmacological properties of cannabis. J Pain Manage 2016;9(4):481-491. https://www.researchgate.net/publication/316545895_The_pharmacological_properties_of_cannabis 2. Mannino J. What is CBD Bioavailability and Why Does It Matter? www.anaviimarket.com https://www.anaviimarket.com/blogs/news/what-is-cbd-bioavailability-and-why-does-it-matter Accessed March 20, 2020. 3. Vučković, Sonja et al. “Cannabinoids and Pain: New Insights From Old Molecules.” Frontiers in pharmacology vol. 9 1259. 13 Nov. 2018, doi:10.3389/fphar.2018.01259 4. Fine PG, Rosenfield MJ. Cannabinoids for Neuropathic Pain. Curr Pain Headache Rep 2014; 18:451-459. doi:10.1007/s11916-014-0451-2.

The onset and duration of cannabis is different based on the mode of administration. The main difference between ingestion and inhalation of cannabis is the delayed onset of action with ingestion. When ingesting cannabis the delayed onset may result in the consumption of a greater than intended amount often resulting in adverse effects but for medicinal cannabis users with chronic conditions, one of the advantages of edibles may be the longer duration of action. Even in states where medicinal cannabis is legal smoking cannabis in public is often still prohibited. 1 The route of administration determines a drug’s pharmacokinetics, Pharmacokinetics is defined as the time and process through which a chemical such as Δ9 -THC, enters the body, travels to various tissues and organs, and is metabolized before elimination. After consuming an edible cannabis product Δ9 -THC is absorbed into the bloodstream and travels via the portal vein to the liver, where it undergoes first-pass metabolism. Liver enzymes (primarily the cytochrome P450 system) hydroxylates Δ9 -THC to form 11-hydroxytetrahydrocannabinol (11-OH-THC). 11-OH-THC is more potent than Δ9 -THC. When cannabis is inhaled through smoking or vaping, Δ9 -THC reaches the brain, takes initial effect within minutes, and shows peak effect in about 20 to 30 minutes, with the psychoactive effects tapering off within 2 to 3 hours. 1 It takes longer for the initial psychoactive effect of edibles (30 to 90 minutes) to be felt, the resulting “high” is longer-lasting, with a peak occurring at 2 to 4 hours after ingestion. The amount of Δ9 -THC in edibles can vary across a single product and across batches formulated at different times, making it difficult for users to estimate how much Δ9 -THC they have consumed Another challenge related to edibles is the cannabis extracts used to produce edibles can be quite different from the actual plant material. There is considerable variation in the amount and homogeneity of cannabinoids in the final product. Since there are no national standards for cannabis labeling. Consumers should receive information about the products they are purchasing that have been tested by a third-party lab. This can help to verify the product's potency, purity, and safety. Consumers should be advised to request the product's certificate of analysis which will provide the consumer with information regarding cannabinoids and terpenes present. their potency in addition to any residual solvents, pesticides, microbial pathogens, and heavy metals present in the product. 2 1. Barrus DG, Capogrossi KL, Cates SC, et al. Tasty THC: Promises and Challenges of Cannabis Edibles. Methods Rep RTI Press. 2016; 2016:10.3768/rtipress.2016. op.0035.1611. doi:10.3768/rtipress.2016. op.0035.1611 2. O’Driscoll A. Why you should read the label on your cannabis product. https://www.leafly.com/news/cannabis-101/how-to-read-cannabis-product-label Published April 30, 2020. Accessed February 27, 2021New Paragraph
